Contents
- 1 hip joint
- 2 Symptoms and diagnosis
- 3 surgical intervention
- 4 The philosophy of the artificial joint among young people
- 5 Tips and recommendations
- 6 Roughness of the knee .. The disease that hardly any home is free of !!
- 7 symptoms and diagnosis
- 8 Treatment plan
- 9 surgical treatment
- 10 artificial knee joint
Hip joint
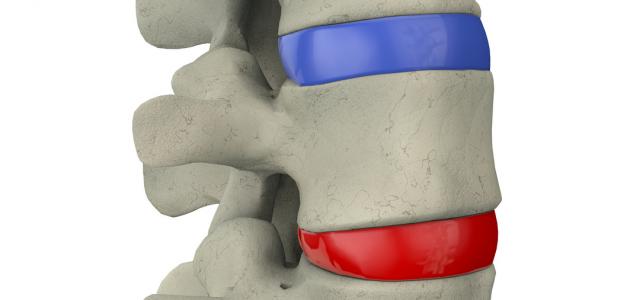
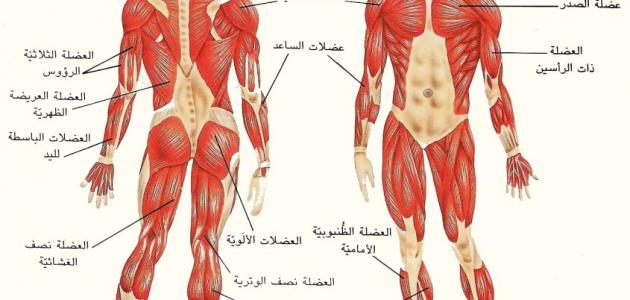
The hip joint is located where the upper part of the thigh bone meets the lower part of the pelvic bone.
This joint is one of the largest joints in the body and provides a great deal of movement needed to carry out normal activities. However, this ... the joint is very sensitive and prone to what is known as congenital sciatic dislocation that occurs in the postpartum period and may not be diagnosed early and leads to the displacement of the upper part of the thigh bone, known as the head of the thigh bone, and its exit from the place where it meets the pelvic bone. This exit causes the leg to be shorter and the range of motion to be reduced. But in some cases in infants, this condition is not diagnosed for one reason or another, which leads to its persistence and leads to other effects.
For example, the joint being in its normal position is very important for normal joint development, and when the joint is outside the normal place, this leads to joint atrophy and the formation of an abnormal secondary joint and the appearance of abnormal movement. When this condition is neglected for many years, the joint is affected and there is stiffness, friction or wear in the hip joint, causing severe pain.
There are other reasons for the occurrence of hip joint roughness other than congenital sciatic dislocation, such as aging or the occurrence of rheumatic diseases such as rheumatoid disease or some blood diseases such as sickle cell disease or some fractures of the thigh bone. Artificial hip joints
Symptoms and diagnosis
In fact, the roughness of the hip joint, whatever its cause, the symptoms are in the form of chronic pain in the hip area, especially from the front at the peritoneum area, which increases over time and increases with movement and when sitting in a squared position and when climbing stairs. These pains may progress to permanent pains even with the slightest movement of the hip joint. In addition, the patient may have trouble walking and obvious lameness. In cases of hip roughness that is due to congenital hip dislocation, there may be a clear shortness of the patient's limb. Usually, the clinical examination reveals this shortness of the lower limb, as well as the presence of limitation in the hip joint and an increase in pain when the doctor moves the hip joint. Then an x-ray of the hip joint is taken that clearly shows the extent of the stiffness and the extent of the displacement of the joint. In some cases, a 3D CT or magnetic resonance imaging may be used.
Joint replacement with an artificial joint
Non-surgical conservative treatment
In all cases, the treatment plan usually begins with conservative methods that consist of avoiding stress, having physical therapy sessions to relieve pain, strengthening the muscles around the hip joint, taking pain medications, muscle relaxants, and anti-inflammatory medications. A medical shoe can also be used to compensate for the shortage in the length of the sick leg in cases of roughness
Resulting from congenital sciatic dislocation. In some cases, topical injection of dipomdrol is used inside the hip joint, which is a needle with a strong anti-inflammatory property that helps relieve pain for different periods ranging from a few weeks to a few months and can be repeated as long as necessary. It can also be sick or ill
Use medical crutches when necessary, especially for long trips.
Surgical intervention
In cases of advanced hip joint osteoarthritis in the elderly or those of forty years or more, the surgical solution is easy in his determination because the best solution is joint replacement with an artificial joint. But the question and confusion usually occur when the patient or patient is young in age, like the case we mentioned earlier. In the past, ten years ago, there was a fear of implanting an artificial hip in young patients, because any artificial joint has a life span. And since the patient is young, he will need to replace the joint and repeat surgery when he reaches the age of forty, for example. For this reason, there is a reluctance to perform these surgeries. Many alternative surgeries for the artificial hip joint have been developed in young people, such as trying to perform surgeries to cover the joint naturally by returning the way the pelvic bone is located to cover the joint. Unfortunately, all of these surgeries have proven their failure to give the patient an adequate amount of rest and also fail to remove symptoms for long periods of time. In addition, during the past ten years there has been a revolution in the development of the quality of artificial hip joints. The new generation of artificial hip joints has become so advanced that the life span of these joints is very long and surpasses the old joints by stages and may last for thirty or forty years, God willing. In addition, the shape of these joints and the way they work has evolved so that all the fears that were associated with the old prosthetic hip joint, such as fear that the artificial joint would dislocate or fear that it would lead to limitation in the movement of the patient or patient and lead to the inability of the patient or The patient sitting on the ground or praying on the ground These fears have disappeared because the new joints have become more stable and give a much greater range of movement than the previous joints, so that the patient can sit on the ground and pray on the ground and practice the activities that a normal person does, God willing. In addition, there is a new generation of artificial joints that cover the parts of the bone without removing the majority of it, and this is considered a great advance that preserves the patient’s bones.
The philosophy of the artificial joint among young people
As mentioned previously, advanced hip joint roughness may occur in the youth group and young people for several reasons, such as congenital hip joint dislocation, rheumatoid disease and blood diseases, sickle cell anemia. This category suffers from severe pain and difficulty in life and difficulty in carrying out normal activities when it is in the prime of life and therefore the effect is doubled, unlike an elderly patient who has achieved most of his ambitions and dreams and his life routine becomes slow and thus the effects of the joint roughness on him are significantly less than the young man who He wants to study, learn, marry, work, and practice sports, as well as a young woman who wants to study, get married, have children, and so on. For this reason, joint osteoarthritis is not only an organic disease, but it also leads to negative psychological effects in these patients. From this standpoint, orthopedic surgeons, especially specialists in joint surgery, have become, during the past few years, frequently performing these operations in this group of young patients.
If we look in depth at which of the two is better. To let the young patient or young patient suffer from pain, limp walking, and the physical and psychological effects of their illness until they grow old, then we perform the surgery. Or that we perform the surgery and save them, God willing, from their pain and from the negative effects of the disease on them, so that they can freely practice various life activities in the youth stage, which is the golden stage. If it is necessary to repeat the joint surgery after twenty or thirty years, so be it
Tips and recommendations
The disease of advanced hip joint osteoarthritis, with all the causes that lead to it, is an unpleasant and painful disease that negatively affects the patient's life, activities and way of life. These negative effects may include the moral and psychological aspect of the patient or patient, especially the youth. And when non-surgical conservative treatment fails to eliminate pain, surgical intervention through the artificial hip joint remains the best and best solution even in the youth group. With the great development in hip joint surgery and modern techniques for these joints, the success rate of this surgery exceeds 90%, God willing. In addition, the life span of the joints became long, reaching twenty to thirty years in most patients. And when this surgery is performed using these modern technologies, the results are excellent in removing symptoms and returning these patients, especially the young, to practice their lives and achieve their aspirations naturally.
Knee roughness .. a disease that hardly any home is free of !!
Surgical intervention may become necessary
A house is not without one or more people who suffer from knee pain, and the most important and most important reason that leads to these pain is knee roughness or what is known as friction, inflammation or erosion of the knee joint, especially in the elderly.
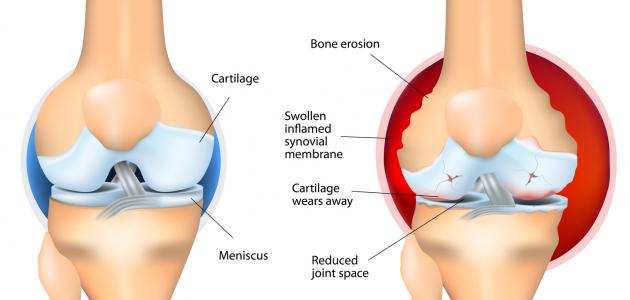
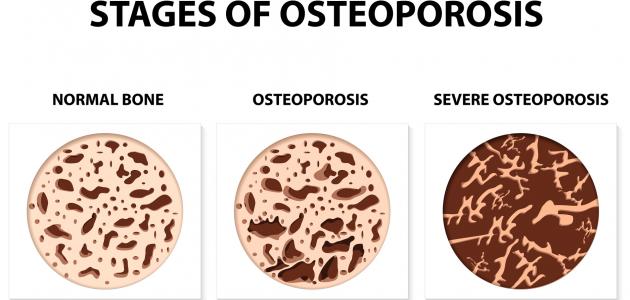
The natural joint, which is located at the meeting of the thigh bone with the shin bone, is covered with a cartilage layer that absorbs shock and provides smooth movement of the joint, but when the amount of this cartilage layer decreases, the resulting disease is what is known as knee roughness, which usually occurs as a result of aging, weight gain, injuries and fractures. Around the knee or as a result of a chronic cut in the cruciate ligament or meniscus, but the most important reasons that lead to the spread of this disease in eastern societies are the habits that lead to stress of the knee joint such as sitting in a squatting position or a squatting position for long periods, lack of fitness, sagging thigh muscles and lack of exercise Sports.
Symptoms and diagnosis
In the initial stages, the patient or the patient complains of pain around the knees or one of them that increases with movement, walking, climbing stairs and stress, and disappears with rest and pain reliever medications, and as the disease progresses, these pains increase in intensity and make daily activities a painful effort such as praying, sitting on the floor and using the bathroom.
This pain is also accompanied by swelling and swelling around the knee joint, stiffness in the movement of the individual and bending, and the feeling of crackling or sounds when moving the joint, but in very advanced cases there may be clear deformation and twisting of the legs and severe difficulty standing and walking even for simple steps.
Although these symptoms may respond to analgesics in the initial stages of the disease, these analgesics become ineffective in the later stages when the roughness has destroyed most of the cartilage, as for the diagnosis, it is by clinical examination and x-rays of the knees in a standing position, These x-rays clearly show the presence of disease and lack of cartilage between the thigh bone and the shin bone, which form the knee joint, as well as the presence of bone growths, joint deformities and sprained legs, and in some cases, magnetic resonance imaging may be required to accurately assess the condition of the cartilage.
Treatment plan
There is no cure or a definitive solution to knee roughness disease, and it is not possible to completely eliminate the disease with treatments. Rather, there is control of symptoms, removal of pain and slowing down the speed of disease progression through an integrated treatment plan consisting of the following:
1- Change in lifestyle, by losing weight, which is one of the most important factors that lead to symptom relief.
In addition, you should exercise light sports such as walking, swimming, light weights, avoid sitting in a squatting and squatting position, not using the Arab bathroom, and praying on a chair when the pain intensifies.
2- Physiotherapy of all kinds, the most important of which is to establish a program to strengthen the front thigh muscles and the knee muscles.
3- Using supportive devices such as walking crutches, medical soft shoes and some types of medical knee bands.
4- Using anti-inflammatory medicines for arthritis and analgesic medicines for pain, by mouth or as topical ointments
5- Using some strengthening proteins that may help restore cartilage, such as (glucosamine) and (chondroitin) pills, which require prolonged use.
6- The use of local needles in the knee joint, such as the (dipomedrol) needle or the (hyaluronate) needle, which helps reduce inflammation and provide a stickiness that helps ease movement within the joint, these needles have temporary effect and need to be repeated every few months.
Surgical treatment
When the conservative treatment plan fails to eliminate the symptoms, surgical intervention is necessary and may consist of the following:
1- Knee arthroscopy: It is an easy operation that is performed through the laparoscope, but its success rate is very small and not permanent in the long term, and it is not recommended in most cases.
2- The process of correcting the curvature of the legs around the knee: It is successful only when the disease is at its onset and when the result of an abnormal twisting of the legs.
Artificial knee joint
A process during which the eroded cartilage is removed and replaced by parts made of titanium metal and high-quality medical plastic plastics, thus eliminating the pain resulting from the friction of the eroded cartilage against each other, and this operation is performed for more than a million patients annually around the world and is considered one of the most successful surgeries Pain and returning patients to practice their normal lives, and although these operations are usually performed in elderly patients who have other health problems such as high blood pressure and diabetes, these problems do not prevent the procedure as it is controlled by sugar and pressure before, during and after The operation, as well as the use of medicines that help prevent complications such as microbial infections or venous thrombosis, and usually the patient spends about seven days in the hospital during which he undergoes physiotherapy sessions during which he learns some exercises that must be observed after discharge from the hospital, and usually the patient can walkWith the help of a physiotherapist on the day after the operation, and the success rate of these operations reaches more than 59%, after which the patient can walk unlimited distances, climb stairs, travel by plane or car, and practice some sports such as walking, swimming, sitting on the floor and sleeping naturally, God willing, and recently, modern technology enabled us From reducing the surgical opening for this operation to about ten centimeters, which helps speed healing and rehabilitation, God willing.
The final advice for patients is to consult a doctor, take full instructions about the procedure, and not hesitate to perform it when non-surgical methods fail to relieve symptoms.