Contents
High intraocular pressure
Ocular hypertension is defined in a simple way as the presence of an actual increase in the pressure inside the eye than normal rates (*), and without this being accompanied by damage to the optic nerve and the appearance of blind spots in the field of vision, and without there being any disease or A specific problem in the eye that causes an increase in intraocular pressure, [1] and here it must be pointed out that the high intraocular pressure requires follow-up with a specialist doctor, as it is a factor that increases the risk of damage to the optic nerve and the individual being infected with glaucoma or glaucoma. It is stipulated that the person who has high intraocular pressure actually suffers from glaucoma requires that the increase in intraocular pressure causes damage to the optic nerve, and a decrease in the field of vision, or that there is a specific cause or disease in the structure of the eye that causes an increase in the pressure inside it. [2] [3]
In fact, there is no clear study of the prevalence of elevated intraocular pressure among people, but it is estimated between 4-10% of the population over the age of forty years, based on a group of large statistical studies. [4] It should be noted that the rise in intraocular pressure It is not accompanied by any initial symptoms or signs that the patient usually notices, until he progresses, and the optic nerve begins to be damaged and damaged, and the symptoms of vision deficiency begin to appear, which is the appearance of blind spots in the side or central parts of the field of vision, and therefore the individual may have a high pressure inside The eye is not aware of this, [5]. The only way to detect the rise in intraocular pressure is to undergo a Tonometry examination with a specialist doctor. Therefore, it is important to visit the ophthalmologist regularly to check on the health and safety of the eyes. [6]
To learn more about high intraocular pressure, read the following article: ( High intraocular pressure and its treatment ) .
Causes of high intraocular pressure
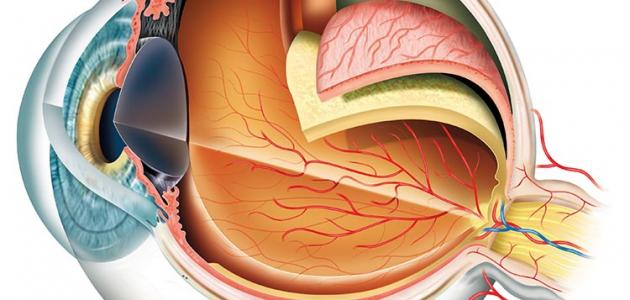
To understand the problem in eye pressure more clearly, it can be said that the eye produces a transparent fluid known as aqueous humor, and this fluid differs from tears. It continuously fills the anterior chambers of the eye, and it works to provide the front parts of the eye that are not directly supplied by blood supply with the necessary nutrients, and to rid them of waste and harmful substances, and in fact this fluid flows through two small chambers at the front of the eye and is drained out of it through drainage channels ( *) The fluid reaches it after crossing the angle at which the iris (the colored part of the eye) meets the cornea (the transparent membrane that covers the iris, the pupil of the eye, and the anterior chamber of the eye) .At the angle where the iris meets the cornea is a spongy tissue known as the trabecular meshwork. (In English:[7] [8]
There are a number of causes and problems that were found to be the cause of high eye pressure, and it is worth noting that the doctor’s discovery of a specific disease or problem that was the cause of high eye pressure in the patient makes him eligible for a medical diagnosis of glaucoma, and the following is a set of these reasons: [3] [9]
- Uveitis: (*) and some other inflammatory eye diseases; Harmful compounds resulting from inflammation can accumulate in the trabecular meshwork and hinder the drainage of the aqueous humor through it, or cause it to become inflamed and blocked, or inflammation causes the drainage angle to close, and chronic inflammation that lasts for an extended period can cause scar tissue to form and increase the disruption of the mixing drainage process. Watery. [10]
- Desquamation or exfoliation syndrome false: ; Which is represented by the accumulation of abnormal proteins in the eye, often at the angle of drainage of the aqueous humor and the trabecular meshwork, which, if it occurs, impedes the ability to drain the aqueous humor. [11]
- Cluttering dye: which is the launching of the pigments of the iris attached in Alterbakah network and hinder the discharge of mixing water. [12]
- Exposure to an eye injury: Whether you were exposed to a direct injury to the eye, it could cause bleeding that obstructs the drainage of the aqueous humor or pushes the iris to close the drainage angle, or an error occurred during a previous eye surgery, especially in retinal detachment operations (*). [12]
- The use of some types of medicines: especially the use of steroid medicines for a long time, as the prolonged use of steroid medicines, whether in the form of drops, eyelid ointments, syrups or oral tablets, injections, or skin patches; It has been observed that steroid drugs can raise intraocular pressure, and if the rise resulting from their use is large and continues for an extended period, it can damage the optic nerve. [13]
- Some congenital problems in the eyes : Congenital abnormalities; Some congenital disturbances in the structure of the eye can be a cause of glaucoma, especially if the problem is represented by a disorder in the optic nerve. [9]
- Some eye lens problems: For example, cataracts or cataracts (*) that affects the lens of the eye, can cause the angle of drainage of the aqueous humor to close in its advanced stages, and thus glaucoma. [12]
- New blood vessels form in the eye: For example, some problems that affect the retina , such as: diabetic retinopathy, and blockage of the central vein of the retina, reduce the retinal blood supply and push the body to form new blood vessels to compensate for the lack of blood supply. It causes an increase in intraocular pressure and closure of the aqueous humor drainage angle. [12]
- Eye tumors: In some cases, a tumor may arise in the eye and affect the angle of drainage of the aqueous humor or cause it to close, raising the intraocular pressure, especially if the tumor originated in the iris, whether due to the large size of the tumor, or it caused the formation of new blood vessels in the eye to obtain Additional feeding, or otherwise. [12]
Factors that increase the risk of high intraocular pressure
It is worth saying that all individuals are susceptible to high intraocular pressure, and this is what prompted the American Academy of Ophthalmology to recommend individuals to undergo a comprehensive eye examination every 5-10 years if they are under 40 years old, and every 2-4 years for age groups between 40-54 years, and every 1-3 years for individuals between the ages of 55-64 years, and every year to two years for individuals over the age of 65 years, but there are factors that make the individual more susceptible to high eye pressure compared to others, and these are recommended to undergo comprehensive eye examinations at a more frequent rate and are advised. By asking the doctor about the regularity rate in the comprehensive eye exams that they should undergo, we mention among these risk factors the following: [14] [15]
- People with a family history of high eye pressure.
- Individuals with diabetes or hypertension.
- Individuals over the age of 40 years.
- People belonging to certain ethnic groups, specifically; African Americans and Hispanics.
- Suffering from Nearsightedness.
Medical follow-up for people with high intraocular pressure
The doctor assesses the eye pressure and other risk factors in the individual that make him more vulnerable to damage to the optic nerve and to developing glaucoma, and accordingly determines whether a person with high intraocular pressure needs treatment to reduce eye pressure or not, and also decides based on these factors the rate of follow-up examinations The regular that the individual should have, which varies greatly from case to case, and it should be pointed out that it is necessary to visit the doctor’s office according to his recommendations, and to undergo the examinations that he recommends because of this great role in effective control of high eye pressure, and to ensure that it does not cause it. With glaucoma, and accelerate treatment of it early in the event that the condition develops, especially since the treatment of glaucoma in its early stages is more effective and contributes to protecting the patient from significant damage to the optic nerve and permanent vision problems that may reach the point of blindness, [16] [17]In general, the most important tests that the doctor regularly conducts to follow up with high intraocular pressure can be stated as follows: [18] [19]
- Examination of the optic nerve: To perform this examination, the doctor places a drop in the patient's eye that expands the pupil, then uses a device that emits light, and contains a magnifying glass, which allows the doctor to examine the optic nerve, and to detect whether it has been exposed to any damage or damage.
- Eye pressure measurement: There are several ways to measure eye pressure, including: Using a microscope known as a slit lamp. To perform the examination, the patient is asked to sit on a chair, and the doctor puts a drop in his eye for local anesthesia, in addition to a specific dye, and then the patient is asked to rest his chin on a specific location in the microscope, and look with the eye through the opening of the microscope, and then the doctor uses an instrument known as an ophthalmometer that allows Estimating the value of intraocular pressure, and it is worth noting that it is recommended to remove contact lenses if an individual uses them before the test because the dye used in the examination can cause permanent staining of contact lenses.
- Square of vision examination: It is a functional examination that tests the patient's field of vision, and checks for the appearance of any problems in the field of vision (on the sides and the center). [16]
______________________________________________________________________________
(*) High intraocular pressure values: It can be said that there is an increase in intraocular pressure if the intraocular pressure exceeds 21 mmHg, after measuring it on two different times, and the individual should be subjected to a central corneal thickness test that affects the accuracy of pressure readings The eye and the doctor's evaluation of it. [20]
(*) Drainage of aqueous humor: the majority of the aqueous humor is discharged through the drainage angle through the trabecular meshwork, meaning that it is the main outlet for the drainage of the aqueous humor, and there is a secondary drainage that drains only a limited amount of the aqueous humor and is known as the solid uveal drainage. [21]
(*) Uveitis: It is known as an inflammation of the middle layer of tissue in the eye wall. Its symptoms usually appear suddenly, and get worse over time, and include blurring of vision, eye pain and redness. [22]
(*) Retinal detachment: which is the detachment of the retina (a thin tissue in the back of the eye) from its location, and it is reported that the detachment of the retina keeps part of its cells away from the blood vessels that supply it with food and oxygen, and it requires immediate treatment. Blindness in the individual, and among its warning symptoms that warn of the need to see a doctor immediately: the sudden appearance of dysfunctions or flashes in the field of vision and lack of vision. [23]
(*) Cataract disease: which is the appearance of dark spots in the lens of the eye, which can cause vision problems such as: blurry or blurred vision, and these symptoms worsen with the passage of time. [24]
References
- ↑ “Ocular Hypertension: New Insights for the Healthcare Professional: 2013 ...” , books.google.jo , Retrieved 08-12-2019. Edited.
- ↑ "Glaucoma" , www.webmd.com , Retrieved 08-12-2019. Edited.
- ^ A b "Ocular Hypertension" , Emedicine.medscape.com , Retrieved 08-12-2019. Edited.
- ↑ "Ocular Hypertension" , emedicine.medscape.com , Retrieved 08-12-2019. Edited.
- ↑ "What is ocular hypertension" , www.aao.org , Retrieved 08-12-2019. Edited.
- ↑ "How is Eye Pressure Measured?" , www.brightfocus.org , Retrieved 08-12-2019. Edited.
- ↑ "Glaucoma" , medlineplus.gov , Retrieved 08-12-2019. Edited.
- ↑ "Aqueous Humor" , www.sciencedirect.com , Retrieved 08-12-2019. Edited.
- ^ A b "Gender : Adult Glaucoma to Suspect" , Www.emedicinehealth.com , Retrieved 08-12-2019. Edited.
- ↑ "Understanding Uveitic Glaucoma" , www.glaucoma.org , Retrieved 12-08-2019. Edited.
- ↑ "Exfoliative Glaucoma" , www.glaucoma.org , Retrieved 08-12-2019.
- ^ A b t w c "Secondary_Glaucoma" , Www.glaucoma-association.com , Retrieved 08-12-2019. Edited.
- ↑ "Glaucoma (steroid)" , www.college-optometrists.org , Retrieved 08-12-2019. Edited.
- ↑ "Ocular hypertension causes" , www.aao.org , Retrieved 08-12-2019. Edited.
- ↑ "Glaucoma" , www.mayoclinic.org , Retrieved 08-12-2019. Edited.
- ^ A b "Ocular Hypertension" , Www.glaucoma-association.com , Retrieved 08-12-2019. Edited.
- ↑ "Ocular Hypertension Treatment & Management" , emedicine.medscape.com , Retrieved 08-12-2019. Edited.
- ↑ "Glaucoma Tests" , medlineplus.gov , Retrieved 08-12-2019. Edited.
- ↑ "Tonometry" , account.allinahealth.org , Retrieved 08-12-2019. Edited.
- ↑ Shibal Bhartiya, Parul Ichhpujani, Clinical Cases in Glaucoma: An Evidence Based Approach , Page 1. Edited.
- ↑ "Aqueous Humor Outflow" , www.ncbi.nlm.nih.gov , Retrieved 08-12-2019. Edited.
- ↑ "Uveitis" , www.mayoclinic.org , Retrieved 08-12-2019. Edited.
- ↑ "Retinal detachment" , www.mayoclinic.org , Retrieved 08-12-2019. Edited.
- ↑ "Cataract Symptoms" , www.webmd.com , Retrieved 4-08-2018. Edited.